Top Tips for Heart Care in Winter: Protect Your Cardiovascular Health from the Cold
Winter brings cold winds, cozy sweaters, and warm drinks—but it also brings increased risks for heart patients. When it comes […]
Winter brings cold winds, cozy sweaters, and warm drinks—but it also brings increased risks for heart patients. When it comes […]
COVID-19 is a rapidly evolving pandemic. Very little is known about it, and most of the information has accumulated from
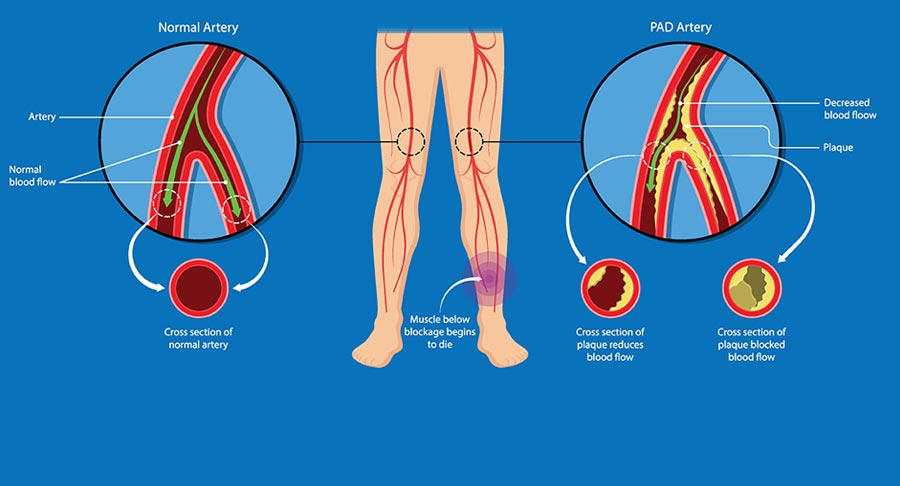
Peripheral arterial disease (PAD) i.e. disease of arteries of the peripheries, is often an unrecognized manifestation of atherosclerosis and other
The electrical activity of your heart is measured by a common, non-invasive test called an electrocardiogram, or ECG. It is helpful in determining the general health of the heart, diagnosing irregular heart rhythms, and looking for evidence of previous heart attacks. To learn more about how your heart works, your doctor may suggest this test if you experience symptoms like palpitations, dizziness, shortness of breath, or chest pain. Electrodes are tiny stickers that are applied to your arms, legs, and chest during the procedure. These electrodes are connected to a device that records electrical impulses from the heart and prints them as a graph. The test is completely painless and typically takes five to ten minutes. Wearing loose clothing can make the electrodes stick more comfortably, but there is no special preparation required. Since the test is non-invasive and doesn’t involve radiation or electricity, there is no risk. You can immediately get back to your regular activities after the test. In order to help you determine whether there are any problems that require attention, Dr. Ahuja goes over the results and explains their significance. Because of this, the ECG is a helpful starting point for assessing heart health.
Angioplasty (Percutaneous Coronary Intervention, or PCI)
Angioplasty, also known as Percutaneous Coronary Intervention (PCI), is a treatment for coronary artery narrowing or blockage, which is frequently brought on by plaque accumulation. Angina (chest pain) or a heart attack may result from reduced blood flow to the heart caused by a blocked artery. A tiny catheter is placed through the skin, typically in the wrist or groin, and guided to the blocked artery during an angioplasty. To increase blood flow and widen the artery, a tiny balloon on the catheter is inflated at the location of the blockage. To keep the artery open, a stent—a tiny metal mesh tube—is usually inserted. Because local anesthesia is used during the procedure, you remain alert but at ease. Usually, the entire procedure takes between thirty and sixty minutes. You must fast for a few hours prior to the procedure, and your prescription may need to be changed. The majority of patients are then monitored for one to two days in the hospital. Although they are uncommon, risks can include artery damage, bleeding, or infection. Dr. Ahuja, however, takes precautions to reduce these risks and frequently uses the wrist approach to promote a speedier recovery. He will ensure that your heart health is safely and effectively managed during the procedure and recovery.
Rotational Atherectomy, or Rotablation
When calcified plaque, or hardened calcium, is obstructing the arteries, rotablation is a technique used during angioplasty. Because hardened plaque may not respond to standard balloon angioplasty, rotablation uses a specialized tool known as a rotational atherectomy. In order to facilitate artery widening and stent placement, this device features a tiny rotating burr that spins quickly to break up tough calcium. Similar to standard angioplasty, the procedure involves inserting a catheter through a tiny incision in your wrist or groin. Rotablation usually needs an experienced team and is saved for extreme situations where other approaches have failed. Fasting in advance is part of the preparation process, and some medications may require adjustments. Dr. Ahuja uses local anesthesia or mild sedation to make sure you’re comfortable throughout the procedure. Although the process typically takes longer than a typical angioplasty, the likelihood of restoring appropriate blood flow is greatly increased. Because of the more intricate work inside the artery, the risks are higher than with a standard angioplasty; however, Dr. Ahuja closely monitors each step. Most patients recover quickly and can return to their regular activities in a matter of days. When other techniques are ineffective, rotablation is a good choice because it guarantees that your arteries are cleared and that blood flow returns.
Atherectomy of the orbits
Angioplasty, also known as Percutaneous Coronary Intervention (PCI), is a treatment for coronary artery narrowing or blockage, which is frequently brought on by plaque accumulation. Angina (chest pain) or a heart attack may result from reduced blood flow to the heart caused by a blocked artery. A tiny catheter is placed through the skin, typically in the wrist or groin, and guided to the blocked artery during an angioplasty. To increase blood flow and widen the artery, a tiny balloon on the catheter is inflated at the location of the blockage. To keep the artery open, a stent—a tiny metal mesh tube—is usually inserted. Because local anesthesia is used during the procedure, you remain alert but at ease. Usually, the entire procedure takes between thirty and sixty minutes. You must fast for a few hours prior to the procedure, and your prescription may need to be changed. The majority of patients are then monitored for one to two days in the hospital. Although they are uncommon, risks can include artery damage, bleeding, or infection. Dr. Ahuja, however, takes precautions to reduce these risks and frequently uses the wrist approach to promote a speedier recovery. He will ensure that your heart health is safely and effectively managed during the procedure and recovery.
Lithotripsy Intravascular (IVL)
A novel treatment for severely calcified coronary arteries, where balloon angioplasty or other methods may not work, is intravascular lithotripsy (IVL). IVL breaks up hard calcium deposits inside the artery by using a catheter that emits shockwaves. The calcium is broken by the shockwaves, which facilitates artery widening and stent implantation. A balloon catheter is frequently used in conjunction with IVL to completely open the artery. Like other angioplasty procedures, the procedure begins with the insertion of a catheter through the wrist or groin. Similar to angioplasty, preparation entails fasting and possibly modifying medication. You will be awake but comfortable during the actual procedure, which is performed under local anesthesia and mild sedation. Dr. Ahuja will insert the catheter into the clogged artery and use controlled shockwaves to break the calcium during the procedure. Although the risks are low, there is a small chance of bleeding, damage to the vessels, or a brief slowdown in blood flow, just like with any procedure. The majority of patients have a brief hospital stay and recover swiftly. In certain situations, IVL has been demonstrated to be both safer and more effective than conventional techniques, and it is especially useful for difficult blockages. Your heart health will benefit from Dr. Ahuja’s proficiency in this procedure.
Intravascular Imaging (IVUS) and OCT
Imaging techniques like intravascular ultrasound (IVUS) and optical coherence tomography (OCT) are used to look inside your arteries during heart procedures like angioplasty. By giving physicians precise images of the arterial walls, these technologies help guarantee that stents are positioned appropriately and that there are no blockages in any of the arteries. While IVUS uses ultrasound and OCT uses light waves, both methods create real-time images of the artery. A catheter is inserted through a tiny incision in your wrist or groin to perform the procedure. The catheter provides a clear view of the artery’s condition as it passes through, enabling Dr. Ahuja to look for plaque accumulation, narrowing, or any areas that require additional care. As with angioplasty, you will get ready for this procedure by modifying your medication and possibly fasting for a few hours. These imaging methods are particularly useful for fine-tuning therapy and guaranteeing proper stent placement. Although there are few risks, the imaging process may cause the procedure to take a little longer than standard angioplasty. By ensuring that everything is done carefully, the information gathered helps to reduce the risk of complications and increase the likelihood of success. In order to help you understand the state of your heart and the next steps in your treatment, Dr. Ahuja will immediately go over the results with you.
Implantation of Pacemakers
A pacemaker is a tiny gadget that is inserted into your body to control a sluggish or erratic heartbeat. It is frequently recommended for those who experience symptoms like fatigue, lightheadedness, or fainting as a result of heart rhythm problems. The pacemaker helps the heart maintain a regular rhythm by sending tiny electrical signals to it. Because local anesthesia and mild sedation are used during the procedure, you will be awake but at ease. Through a tiny incision, Dr. Ahuja places the pacemaker beneath the skin close to your collarbone. The pacemaker then connects to the heart by means of thin wires, or leads, that are inserted into the heart through veins. A hospital stay of one to two days is typically necessary for monitoring after the procedure, which takes around one to two hours. You may need to modify some of your medications and fast for a few hours prior to the procedure. Although the risks are minimal, they may include infection or swelling at the implant site. Although lifting heavy objects should be avoided at first, most people recover from the implantation quickly and can return to their regular activities within a week. Dr. Ahuja will go over how the pacemaker works and how it can improve your quality of life by keeping your heartbeat steady. In order to ensure your pacemaker continues to function properly over time, he will also help you with follow-up care.
Implantable cardioverter defibrillator (ICD)
Similar to a pacemaker, an implanted cardioverter defibrillator (ICD) shocks the heart if it begins to beat dangerously quickly or abnormally. ICDs are frequently advised for people who have heart failure or irregular heart rhythms that put them at high risk of sudden cardiac arrest. Implanting an ICD is similar to implanting a pacemaker. Dr. Ahuja places the device beneath your skin, close to your collarbone, and connects it to your heart through tiny veins. The ICD continuously tracks the rhythm of your heart after it is implanted. It will shock the user to return the heartbeat to normal if it detects a dangerously irregular one. You will stay in the hospital for one to two days for observation after the procedure, which typically takes one to two hours. Fasting is part of the preparation, and you’ll need a ride home afterward. Although the risks are low, they could include discomfort, swelling, or infection at the implant site. You will need routine examinations following the procedure to make sure the device is operating as intended. Knowing that their heart is being watched over constantly reassures most patients. To give you peace of mind that your heart is protected, Dr. Ahuja will go over the specifics of how the ICD works and what to do in the event that the device shocks you.
Cardiac Resynchronization Therapy (CRT-P/CRT-D)
People with severe heart failure, in which the left and right sides of the heart do not beat in unison, benefit from cardiac resynchronization therapy, or CRT. The heart’s capacity to pump blood efficiently may be weakened by this asynchrony. With CRT, a device that helps the heart beat together by sending electrical signals to both sides is implanted. There are two varieties of CRT: CRT-D, which can shock if necessary, and CRT-P, which functions similarly to a pacemaker. Local anesthesia and mild sedation are used during the procedure, which is comparable to pacemaker implantation. Dr. Ahuja places leads in the heart and inserts the device through a tiny incision close to the collarbone. You will remain in the hospital for one to two days for observation, and the procedure usually takes two to three hours. Medication adjustments and fasting are part of preparation. Although there are usually few risks, infection or swelling at the implant site are possible side effects. The majority of patients report notable symptom improvements following implantation, including less exhaustion and dyspnea. In addition to giving you advice on how to manage your heart condition going forward, Dr. Ahuja will modify the device to ensure that your heart beats as efficiently as possible.
Transcatheter Aortic Valve Replacement (TAVR)
A damaged or narrowed aortic valve in the heart can be replaced with TAVR, a minimally invasive procedure. People who are unable to undergo traditional open heart surgery because of their age, frailty, or other medical conditions are typically advised to choose this option. A tiny incision is made in the chest or groin to perform the procedure. The heart is expanded to replace the old valve after a replacement valve is inserted via a catheter. You will be under general anesthesia during the one to two-hour procedure. To make sure the new valve is positioned correctly, Dr. Ahuja and the cardiac team will keep a close eye on the process. Fasting is part of the preparation, and you might have to have a number of imaging tests done first. You will need to recuperate in the hospital for two to five days following the procedure. Compared to traditional surgery, TAVR has fewer complications and offers a quicker recovery. Although the risks are minimal, they could include stroke, infection, or bleeding. After that, the majority of patients report a notable improvement in symptoms like exhaustion or shortness of breath. From pre-surgery imaging to post-surgery care, Dr. Ahuja will make sure you are completely supported at every stage.
Endovascular Aortic Aneurysm Repair (EVAR/TEVAR)
The large artery that transports blood from the heart to the rest of the body, the aorta, has bulging sections called aneurysms that can be fixed with minimally invasive procedures called EVAR and TEVAR. Aneurysms in the abdominal aorta are treated with EVAR, whereas those in the thoracic (chest) region are treated with TEVAR. In both procedures, a stent graft is inserted through a tiny incision in the groin and guided into place using a catheter. Once in position, the stent graft aids in strengthening the aorta’s weak spot and keeps it from rupturing. Under general anesthesia, the procedure usually takes one to two hours to complete. Imaging tests such as CT scans to map the aneurysm are part of the preparation process, and you might need to fast beforehand. Following the procedure, you will typically remain in the hospital for one to two days for monitoring. Despite the possibility of bleeding or infection, it is much less invasive than traditional surgery, which speeds up recovery. The majority of patients get better in a few weeks and are able to resume their regular activities. In order to help you manage your recuperation for the best result, Dr. Ahuja will carefully assess your condition and select the most effective technique to repair the aneurysm.
Myocardial Perfusion Imaging, or Stress Nuclear Scan
Myocardial Perfusion Imaging, also known as a Stress Nuclear Scan, evaluates the flow of blood to your heart muscle under stress and at rest. It is frequently used to assess the degree of coronary artery disease, or blocked arteries, or to monitor the effectiveness of heart surgery such as bypass or angioplasty. A tiny quantity of a radioactive tracer is injected into your bloodstream during the test. Images of your heart at rest and after stress—which may result from treadmill exercise or medication—are then captured by special cameras. Finding the parts of your heart that receive less blood flow is made easier with the help of the tracer. On test day, preparation entails avoiding caffeine and fasting for a few hours. Since pictures are taken both at rest and after stress, the test typically takes several hours to finish. There are very few risks and very little radiation exposure. This test gives Dr. Ahuja vital information about how your heart is working, which he can use to develop a targeted treatment plan that may include medication, lifestyle modifications, or more involved procedures.
Myocardial Viability PET Scan
A specialized test called a PET scan for myocardial viability determines whether heart muscle that has been weakened by decreased blood flow is still viable and can recover with treatment. People with heart failure, in which certain heart muscles do not function properly, should pay special attention to this test. A radioactive tracer is injected into your bloodstream during the scan. A specialized camera takes pictures of your heart after it has had time to circulate. Areas that are still alive and could recover with improved blood flow are highlighted by the tracer. For best results, preparation entails fasting and adhering to a particular diet in advance. Although the scan is painless, it could take an hour or so to finish. Because of the minimal radiation exposure, this procedure is safe. Following the scan, Dr. Ahuja will use the results to inform treatment choices, including whether weak heart muscle could be restored through procedures like angioplasty or bypass surgery. For people with heart failure, this test provides useful information that helps them decide how best to improve their heart health.